FOR IMMEDIATE RELEASE
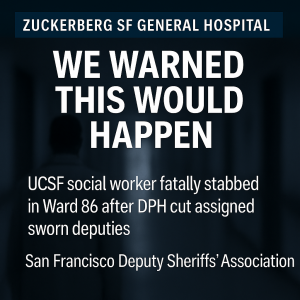
San Francisco Deputy Sheriffs’ Association: Stabbing of Social Worker at Zuckerberg San Francisco General Was Predictable — and Preventable
Union calls on City leaders to restore deputy sheriff staffing on high-risk units after years of documented assaults and ignored warnings
San Francisco, CA — On December 4, 2025, a 31-year-old UCSF social worker was repeatedly stabbed by a patient in Ward 86 at Zuckerberg San Francisco General Hospital (ZSFGH) and left in critical condition. The San Francisco Deputy Sheriffs’ Association (DSA) says this tragedy is exactly what deputies and staff warned would happen when the Department of Public Health (DPH) cut deputy sheriff positions and shifted to a “response-only” security model.
“This was not a random, unforeseeable incident,” said DSA President Ken Lomba. “ZSFGH’s own data show years of serious assaults and weapons on campus. Deputies, nurses, and social workers told DPH that pulling deputies off high-risk units/posts and replacing them with unarmed cadets and distant response teams would get someone seriously hurt or killed. On December 4, that prediction came true.”
A uniquely high-risk safety-net hospital
 Zuckerberg San Francisco General is San Francisco’s only Level 1 trauma center and the city’s only 24/7 psychiatric emergency department, serving roughly 100,000 patients a year and treating nearly 4,000 severely injured trauma patients annually, including gunshot wounds, stabbings, and other violent assaults.
Zuckerberg San Francisco General is San Francisco’s only Level 1 trauma center and the city’s only 24/7 psychiatric emergency department, serving roughly 100,000 patients a year and treating nearly 4,000 severely injured trauma patients annually, including gunshot wounds, stabbings, and other violent assaults.
Unlike Los Angeles County or Alameda County, which spread trauma and psych-emergency patients across many hospitals, San Francisco relies on one safety-net campus for residents of San Francisco and northern San Mateo County. That means gunshot victims, stabbing victims, high-risk psychiatric emergencies, and people in severe crisis all converge on a single crowded hospital, placing an unusually heavy safety burden on deputies and clinicians working there.
ZSFGH’s own internal data show that violence has been a persistent problem:
-
Between January 1, 2020 and September 30, 2021, ZSFGH recorded 748 workplace violence events, including 303 incidents in the Emergency Department and 215 in psychiatry units alone.
-
The hospital’s Security Annual Report for FY 2020-2021 notes that deputies responded to 13,339 patient-related security calls, confiscated 3,394 weapons and contraband at Emergency Department screening, and investigated 23 moderate or high-risk workplace-violence threats.
-
ZSFGH’s FY 2024-2025 Annual Report shows that even after new training and prevention initiatives, the hospital still averaged six physical assaults with injury each month across just five high-risk areas, barely below the prior-year baseline of seven assaults with injury per month and far above the hospital’s target of fewer than four.
Despite these red flags, DPH moved forward with a restructuring that reduced deputy sheriffs on campus and clinics, expanded unarmed cadet roles, and relied more heavily on distant response teams and behavioral-health staff to manage escalating violence.
December 4, 2025: Exactly what staff warned would happen
On December 4, 2025, hospital staff had already raised safety concerns about a patient and requested deputy protection for a doctor at Ward 86 who had received threats. While the deputy was in a nearby room providing security for the threatened doctor, he heard a disturbance and saw the same patient in the hallway repeatedly stabbing a 31-year-old UCSF social worker with a kitchen knife, inflicting multiple wounds to the neck and shoulder.
He immediately went into the hallway, restrained the suspect, and allowed medical staff to begin CPR and lifesaving measures.
Research on close-range knife attacks (often summarized as the “21-foot rule”) shows that an assailant can cover about 21 feet in roughly 1.5 seconds—about the same time it takes a trained officer to perceive the threat and react—meaning a determined attacker can deliver multiple stab wounds in the one to two seconds before even a nearby responder can physically intervene. In a response-only model where deputies are stationed elsewhere on campus, that delay is far longer. By the time help arrives from another building or floor, a victim may already have sustained fatal injuries.
“This is exactly why we opposed a ‘civilian roving response team’ model for a hospital like ZSFGH,” Lomba said. “Knife attacks happen in seconds. If a deputy is on the opposite side of the campus when an employee is attacked on an upper floor, the response time is so long that the employee could be dead before help arrives. On December 4, a deputy happened to be close enough to intervene—and even then, the social worker suffered life-threatening wounds.”
The deputy who saved a life
The DSA recognizes the responding sheriff’s deputy as a hero for his actions on December 4. While providing security for a threatened doctor in Ward 86, he heard a disturbance, saw the social worker being repeatedly stabbed, and immediately intervened, restraining the attacker and securing the scene. His rapid response allowed medical staff to begin CPR and other lifesaving measures within moments, giving the victim a fighting chance to survive injuries that could easily have been fatal.
“This is exactly what deputy sheriffs are supposed to do on high-risk units: be close enough to stop an attack in progress and protect frontline healthcare workers,” Lomba said.
DPH was warned in 2022
In 2022, during a video-conference meeting with DPH and ZSFGH leadership, DSA President Ken Lomba objected to Security Director Basil Price’s plan to reduce deputy sheriffs and rely more heavily on cadets and civilian staff paired with social workers.
Lomba explained that the proposed security model was copied from Los Angeles County and would not work in San Francisco’s environment, where there is only one Level 1 trauma and psych-emergency hub and far fewer sworn officers available across the city. In contemporaneous notes and texts summarizing his comments to DPH leaders, Lomba warned that reducing deputies would:
-
Turn ZSFGH into a “reaction-only” scene,
-
Leave staff and patients exposed during the first critical seconds of an attack, and
-
Create scenarios where “if a deputy is on the opposite side of campus and an employee gets attacked or stabbed on an upper floor or roof of SFGH, the response time would be so long the employee could be dead.”
Lomba’s concerns echoed what deputies and security staff had been documenting in workplace-violence and crime reports for years: moving deputy sheriffs off units and treating ZSFGH as a campus that can be secured by unarmed cadets and roaming response teams would increase response times and leave employees unprotected during the most dangerous moments of an attack.
Nonetheless, DPH proceeded with a model that reduced deputy sheriffs on campus, leaving fewer deputies responsible for a large hospital campus and stationed farther away from high-risk wards—including Ward 86—while publicly emphasizing new training, behavioral-health teams, and technology upgrades.
ZSFGH’s own reports acknowledge ongoing assaults
In recent annual reports, ZSFGH acknowledges that workplace violence “continues to be a serious challenge” and that healthcare workers are nearly four times more likely than workers in most other industries to experience workplace violence.
The hospital highlights a campus security assessment, weapons detection systems, de-escalation training, the Behavioral Emergency Response Team (BERT), and an Assault Governance Task Force, and sets a goal of reducing assaults with injury in high-risk areas.
Yet the FY 24-25 data show that even after these initiatives, staff are still suffering, on average, six assaults with injury every month in just five high-risk areas—a level of violence that underscores the need for immediate, on-scene protection, not only after-the-fact response.
What must change now
The San Francisco Deputy Sheriffs’ Association calls on DPH, the Health Commission, and the Mayor to take the following immediate steps:
-
Restore and increase deputy sheriff positions on high-risk units, in behavioral-health settings, vehicle/foot patrol and in HIV/positive-health clinics, rather than relying on distant response teams and unarmed cadets.
-
End the experiment of replacing deputies with unarmed cadets and civilian staff in roles that routinely face violent, armed, or unstable patients. Cadets and civilians can play a valuable supportive role, but they cannot safely substitute for trained, sworn law-enforcement officers in high-risk environments.
-
Convene a joint hospital safety task force that includes deputies, nurses, social workers, physicians, and patient advocates to design a security model grounded in real-world response times, the physics of close-quarters attacks, and the hospital’s own workplace-violence and crime data.
-
Fully integrate workplace-violence and security metrics into hospital governance, including transparent reporting on assaults, weapons confiscated, and use-of-force, and clear accountability when staffing or policy decisions increase risk.
“ZSFGH’s own reports show a hospital that has been struggling with workplace violence for years while trying to manage an extraordinarily high-risk patient population,” Lomba said. “Our deputies are proud to protect this campus, but they cannot do it from across town or across campus. The City must put deputy sheriffs back where the danger is—on the units, in the clinics, and at the front doors—before another nurse, doctor, or social worker pays the price.”
Until ZSFGH recognizes that violence can unfold in seconds and structures security around prevention and immediate intervention—not delayed response, frontline staff and patients will remain at unacceptable risk.
Media Contact:
San Francisco Deputy Sheriffs’ Association
415-696-2428 • SanFranciscoDSA.com